On Pins & Needles: Acupuncture Appears to Help with Alcohol Use Disorder
Acupuncture emerged as a treatment for addiction over 40 years ago – yet studies determining its effectiveness for substance use disorders have been lagging. There are only a few randomized controlled trials that have analyzed the potential benefits of acupuncture for alcohol use disorder symptoms. However, in aggregate, they suggest a small benefit in terms of relief from craving during recovery.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
There is a strong appeal for complementary and alternative medicine across many disorders and some evidence to suggest its utility in substance use disorders (Grant et al 2016). Though the number of studies examining the role for acupuncture in alcohol use disorders has been small, looking at these studies in aggregate allows stronger conclusions to be drawn about its potential role in treatment, and to identify scientific gaps to inform future work in the area.

HOW WAS THIS STUDY CONDUCTED?
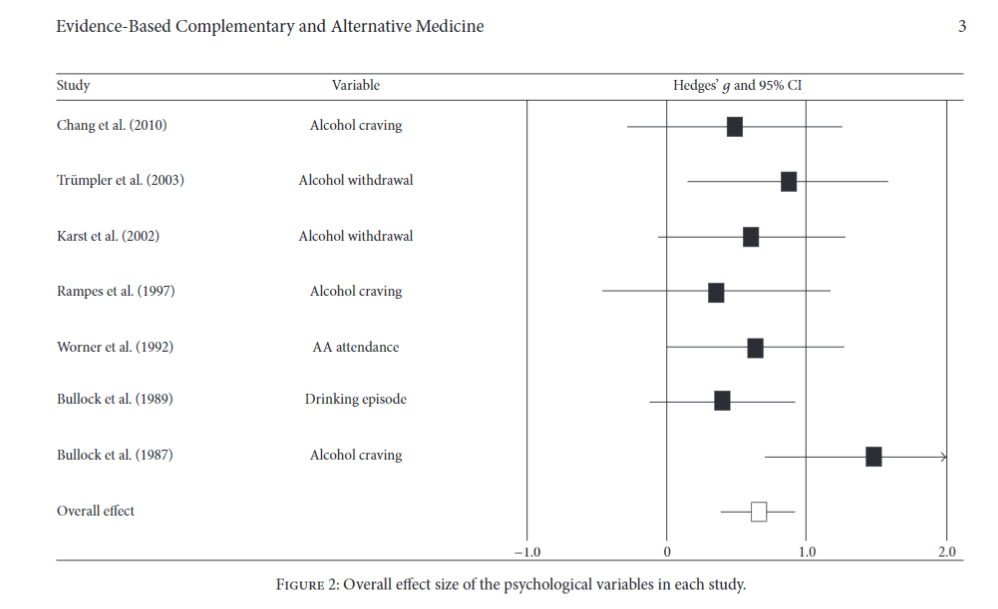
A scientific literature review through August 2016 was conducted searching for articles including both acupuncture and alcohol terms. Of the original 806 articles collected, seven studies (totaling 243 participants) were identified meeting the inclusion criteria (randomized controlled trials assessing the effects of acupuncture on individuals with a primary alcohol problem reporting statistics in peer-reviewed English-language journals). The data reported was converted to effect sizes for the last time point (with n>10 subjects) included. The psychological variables assessed include alcohol craving, alcohol use and anxiety with at least three studies including for each psychological variable.
Any follow-up data was also extracted (only two studies reported six month data and only one had twelve month post-treatment data). Data is reported as Hedges’ g representing the difference of the means for acupuncture and control conditions divided by the pooled standard deviation and corrected for small sample size biases.
WHAT DID THIS STUDY FIND?
The overall effect size across the seven studies was medium: (g = 0.67) in favor of acupuncture over control across the various psychological measures (alcohol craving, withdrawal, AA attendance, drinking episodes). When the analysis is limited to alcohol cravings or alcohol use, the effect size increases (g = 0.78). No difference was found between acupuncture and control with regard to anxiety measures (g = 0.). When the three studies collecting longer-term data (six and twelve month follow-ups) were examined, the effect size in favor of acupuncture was small but statistically significant (effect size = 0.286).
SOURCE: (Shin et al., 2017)
The heterogeneity of the studies included confounds the effect sizes described: The above finding is in the context of a small number of studies with quite variable acupuncture/control protocols and outcome measures, so detecting any effect size changes is challenging. Some studies only included acupuncture on the ear (a newer form of acupuncture known as auricular acupuncture) and others only acupuncture on the traditional Chinese medicine meridian points along the body; some studies had placebo needles, others had no needles as a control.
The authors attempted to control for heterogeneity (using a Q test) which showed that heterogeneity was minimal for the overall effect, but significant for some measures, including alcohol craving and alcohol use. These latter two measures showed the largest beneficial effects of acupuncture, so the magnitude of the finding is likely less than that reported due to the variations in the data included.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
There is insufficient data thus far to convincingly demonstrate the beneficial effects of acupuncture for recovery from alcohol use disorder. However, the data nonetheless points to a positive effect that is statistically significant across various studies. Given the low side effect burden and desirability of acupuncture, even a small effect might broaden the number of modalities that those with alcohol use disorder can pursue to aid recovery.
This study is generally congruent with a previous meta-analysis on acupuncture and substance use disorders – This larger prior study (41 studies and 5,227 participants) identified a difference in favor of acupuncture for reducing substance withdrawal/cravings symptoms (SMD -0.57) and for reducing anxiety (SMD -0.74) but did not show differences in relapse or substance use. They reported that publication biases reduce the magnitude of the effects they did find, similar to the study presented. This prior study found that traditional Chinese medicine acupuncture had a better effect than auricular acupuncture on withdrawal/craving symptoms, whereas this current study included more auricular acupuncture studies.
- LIMITATIONS
-
- The number of studies included was small (seven) with only 243 participants. Given the different outcome measures used, this means that there were exceedingly few studies pooled per outcome measure.
- The acupuncture and control treatments pooled varied considerably – five studies had only auricular acupuncture, two had body stimulation points, four studies had placebo needle or another intervention, and treatment length varied from 15-45 minute sessions over two weeks to three months.
- The authors report significant heterogeneity for alcohol cravings and alcohol use, the two measures that showed the largest effect sizes. They did not then attempt to take into account that heterogeneity to determine how much the effect size would be reduced by.
- Given the number of variables they looked it, and the modesty of the findings, there is a need for larger randomized controlled studies to more conclusively show whether acupuncture has a reproducible effect on alcohol use disorder symptoms.
BOTTOM LINE
- For individuals & families seeking recovery: Although the data is not overwhelmingly conclusive in favor of acupuncture for alcohol use disorder, it is suggestive that acupuncture may reduce symptoms of withdrawal and perhaps reduces alcohol use and that these effects may be sustained over the following months. It is always useful to consider additional and complementary treatments to help sustain abstinence and acupuncture seems to help with no evidence that it detracts from recovery.
- For scientists: Larger randomized controlled trials are needed to test the effects of acupuncture (and other complementary approaches) on recovery from substance use (especially as compared with other more established treatments). This study suggests that an internal comparison of traditional Chinese acupuncture vs. auricular acupuncture may also be beneficial.
- For policy makers: Once (or if) the benefit of complementary approaches such as acupuncture are convincingly demonstrated for substance use disorders, then encouraging insurance companies to partially reimburse for these services would aid in increasing the treatment modalities available to those in recovery. However, a cost effectiveness analysis of the relative costs of complimentary approaches on achieving beneficial outcomes would be a key factor in determining whether the desirability of increasing access to this approach (it is likely cheaper than medical approaches but also less effective so cost-benefit analyses would be important to pursue).
- For treatment professionals and treatment systems: Working with patients to identify the array of treatments that might aid in their recovery is beneficial on many levels. Increasing awareness about the modalities that show some promise is helpful even if the data is not sufficiently strong to rely on just acupuncture just yet.
