What If Cost was Not a Factor in Accessing Substance Use Disorder Treatment?
Sweden has a universal healthcare system that includes unlimited, free substance use disorder (SUD) treatment.
Although a mixed set of findings, some researchers suggest a follow-up episode of care may be a step toward recovery.
Few studies have examined what factors influence engaging in multiple episodes of care. Due to its privatized system, researchers in the United States are unable to separate the impact of clinical need from personal healthcare resources (e.g., insurance) on treatment seeking.
Furthermore, women account for roughly 32% of SUD treatment admissions, though we are only beginning to learn about their unique clinical and recovery needs. Motherhood in particular is a valuable area in recovery research because the most common ages to seek SUD treatment (young adulthood) overlap with the most likely ages where a woman has young children or will become pregnant. Researchers in other areas have shown a plethora of lasting, deleterious effects of SUD on maternal and child health during pregnancy and early life.
For example, in US samples, poverty is a strong risk factor for the development of SUD. This same factor of poverty as asks a barrier to insurance and treatment.
To examine what factors might predict treatment seeking in a system where SUD treatment is universally available and whether those are qualitatively different from factors influencing treatment seeking in the US, Grahn and colleagues identified several predisposing (e.g., gender), enabling (e.g., education) and need factors (e.g., clinical severity) associated with history of voluntary SUD treatment episodes for a national sample of 12,009 treatment-seeking adults who had an average of 4.3 treatment episodes.
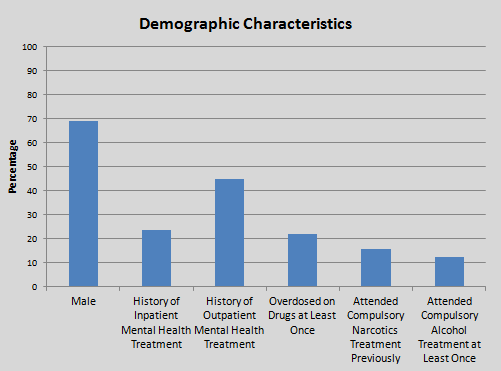
Study participants were 40 years old and had 11 years of education on average, 69.1% male, with 11 years of education on average. Mental health treatment seeking was also common; 23.6% had received inpatient and 44.8% received outpatient treatment.
Clinically, patients with greater substance use severity, including number of mandated treatment episodes, alcohol and drug scores on the Addiction Severity Index and years with 3 or more days per week of substance use to intoxication/impairment, and psychiatric severity (including symptoms and history of inpatient treatment), and higher ASI alcohol score, predicted more voluntary treatment episodes. Interestingly, immigration status and education did not predict number of treatment episodes. Generally, findings here are consistent with others showing individuals with the greatest need access treatment more often.
IN CONTEXT
Despite differences in healthcare models between Sweden and the US, the findings here could be generalized to those in the US which suggests that individuals with more severity are more likely to seek treatment. Of note, however, is that the trends described above were quite small.
This suggests they are reliable (consistent) but may not be clinically meaningful. Of those meeting the field’s criteria for at least a small effect – allowing us to assume some practical significance – years of regular substance use, history of mandated treatment, prior inpatient mental health treatment, and having been charged with a crime remain salient indicators of repeated SUD treatment seeking.
Taken together, the data here suggest, particularly for individuals with greater severity, it may behoove third-party payers to conceptualize recovery from addiction in context of an overall management plan that often includes multiple episodes of treatment and ideally includes support for post-treatment continuing care.
CITATIONS
Grahn, R., Chassler, D., & Lundgren, L. (2014). Repeated addiction treatment use in Sweden: A national register database study. Substance use & misuse, 49(13), 1764-1773.
